The integrative model of mood disorders shows that a comprehensive understanding of mood disorders requires considering biological, psychological, and social factors. This model provides a framework for understanding the complex interplay of these factors and their implications for treatment planning.
The integrative model has its roots in the biopsychosocial model of health and illness, which emphasizes the interconnectedness of biological, psychological, and social factors in health and disease. The integrative model of mood disorders applies this biopsychosocial perspective to the specific case of mood disorders, offering a comprehensive framework for understanding their etiology, diagnosis, and treatment.
The Integrative Model of Mood Disorders: An Overview
The integrative model of mood disorders provides a comprehensive framework for understanding the etiology, diagnosis, and treatment of mood disorders. This model recognizes the complex interplay of biological, psychological, social, and environmental factors in the development and maintenance of these disorders.
Key Components and Principles, The integrative model of mood disorders shows that
The integrative model is based on the following key components and principles:
- Mood disorders are multifactorial, resulting from the interaction of multiple risk factors.
- Biological, psychological, social, and environmental factors all contribute to the development and course of mood disorders.
- The model emphasizes the importance of a holistic approach to assessment and treatment.
- Treatment should be tailored to the individual needs of the patient.
Historical Development and Theoretical Underpinnings
The integrative model of mood disorders has its roots in the work of early psychiatrists and psychologists who recognized the importance of both biological and psychological factors in mental illness. In the 1950s and 1960s, researchers began to develop more sophisticated models of mood disorders that incorporated a broader range of factors.
The integrative model emerged as a comprehensive synthesis of these earlier models.
Biological Factors in Mood Disorders
Neurotransmitters and Brain Structures
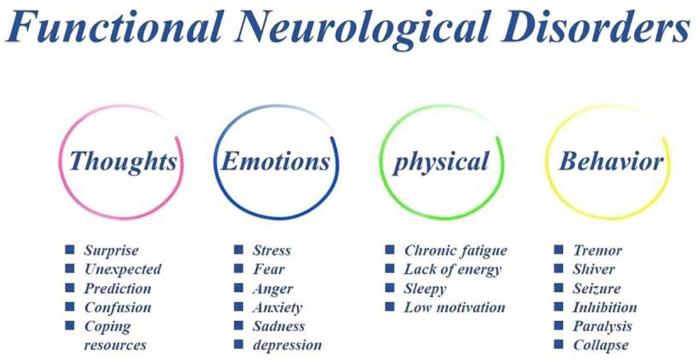
Neurotransmitters are chemicals that transmit signals between neurons in the brain. Several neurotransmitters, including serotonin, norepinephrine, and dopamine, have been implicated in the regulation of mood. Imbalances in these neurotransmitters can contribute to the development of mood disorders.
Certain brain structures, such as the amygdala and hippocampus, are also involved in mood regulation. Abnormalities in these structures have been linked to the development of mood disorders.
Genetic and Epigenetic Factors
Mood disorders have a strong genetic component. Studies have identified several genes that are associated with an increased risk of developing a mood disorder. However, it is important to note that genetic factors alone do not determine whether or not someone will develop a mood disorder.
Epigenetic factors can also play a role in the development of mood disorders. Epigenetics refers to changes in gene expression that do not involve changes in the DNA sequence. These changes can be caused by environmental factors, such as stress or trauma, and can have a lasting impact on brain function.
Hormonal Imbalances and Physical Health Conditions
Hormonal imbalances can also contribute to the development of mood disorders. For example, thyroid problems and imbalances in sex hormones can lead to changes in mood. Physical health conditions, such as chronic pain or cancer, can also have a negative impact on mood.
Psychological Factors in Mood Disorders
Cognitive and Behavioral Factors
Cognitive and behavioral factors play a significant role in the development and maintenance of mood disorders. Negative thinking patterns, such as rumination and catastrophizing, can contribute to low mood. Maladaptive coping mechanisms, such as avoidance and substance abuse, can also worsen mood symptoms.
Stress, Trauma, and Life Events
Stress, trauma, and life events can all trigger mood disorders. Stress can activate the body’s fight-or-flight response, which can lead to changes in mood, sleep, and appetite. Trauma can have a lasting impact on brain function and can increase the risk of developing a mood disorder.
Interpersonal Relationships
Interpersonal relationships can also affect mood. Supportive relationships can buffer against stress and improve mood, while negative relationships can worsen mood symptoms.
Social and Environmental Factors in Mood Disorders

Social Support and Social Isolation
Social support can have a positive impact on mood. People with strong social networks are more likely to recover from mood disorders and have better long-term outcomes. Social isolation, on the other hand, can increase the risk of developing a mood disorder.
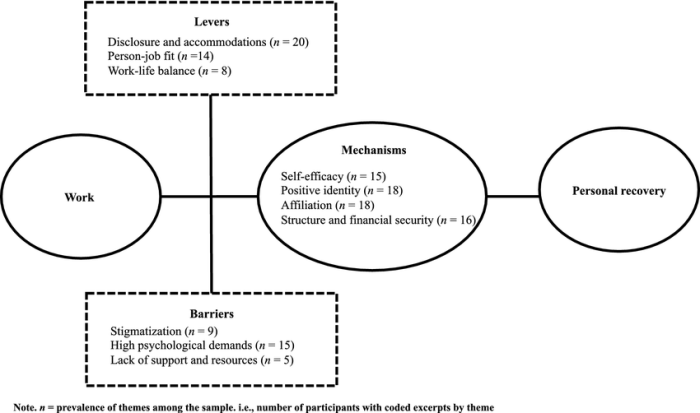
Socioeconomic Status and Occupational Stress
Socioeconomic status and occupational stress can also affect mood. People with low socioeconomic status are more likely to experience poverty, discrimination, and other stressors that can contribute to the development of a mood disorder. Occupational stress can also lead to burnout and other mental health problems.
Environmental Stressors
Environmental stressors, such as pollution, noise, and overcrowding, can also have a negative impact on mood. These stressors can activate the body’s stress response and lead to changes in mood, sleep, and appetite.
Stigma and Discrimination
Stigma and discrimination can also worsen mood symptoms. People with mood disorders may be afraid to seek help because of the stigma associated with mental illness. This can lead to delayed diagnosis and treatment, which can worsen the course of the disorder.
Treatment Implications of the Integrative Model
Treatment Planning
The integrative model of mood disorders has important implications for treatment planning. The model emphasizes the need for a holistic approach to assessment and treatment. This means that clinicians should consider the biological, psychological, social, and environmental factors that may be contributing to the patient’s mood disorder.
Therapeutic Interventions
The integrative model can guide the selection of therapeutic interventions. For example, a patient with a mood disorder that is primarily caused by biological factors may benefit from medication. A patient with a mood disorder that is primarily caused by psychological factors may benefit from psychotherapy.
A patient with a mood disorder that is caused by a combination of biological and psychological factors may benefit from a combination of medication and psychotherapy.
Role of Psychotherapy, Medication, and Lifestyle Modifications
Psychotherapy, medication, and lifestyle modifications are all important components of treatment for mood disorders. Psychotherapy can help patients to identify and change negative thinking patterns and behaviors. Medication can help to regulate neurotransmitter imbalances and improve mood. Lifestyle modifications, such as exercise, diet, and sleep hygiene, can also improve mood and reduce the risk of relapse.
Top FAQs: The Integrative Model Of Mood Disorders Shows That
What are the key components of the integrative model of mood disorders?
The key components of the integrative model of mood disorders include biological factors (e.g., neurotransmitters, brain structures, genetics), psychological factors (e.g., negative thinking patterns, maladaptive coping mechanisms, interpersonal relationships), and social factors (e.g., social support, social isolation, cultural factors).
How does the integrative model of mood disorders differ from other models of mood disorders?
The integrative model of mood disorders differs from other models in that it considers the interplay of biological, psychological, and social factors. Other models may focus on one or two of these domains, but the integrative model recognizes that all three domains are important in understanding and treating mood disorders.
What are the implications of the integrative model of mood disorders for treatment planning?
The integrative model of mood disorders suggests that effective treatment should address all three domains of biological, psychological, and social factors. This may involve a combination of psychotherapy, medication, and lifestyle modifications.